Periodic Checkup by an ophthalmologist is the only means to Preserve Vision
A healthy retina is necessary for proper vision. The amount of light entering the eye is controlled by the iris and is then passed to the retina. The retina is a thin membranous lining at the back of the eye. It is a light-sensitive nerve tissue that controls how images are viewed. The images are focused here and converted to electrical impulses which are carried to the brain by the optic nerve.
Diabetic Retinopathy
The most common eye complication in diabetes is diabetic retinopathy; the other complications are cataract and glaucoma.Early detection and timely treatment of diabetic eye disease significantly reduces risk of vision loss. Diabetic retinopathy produces visual symptoms only when it is very advanced. Since only an ophthalmologist can detect early signs of diabetic retinopathy, all diabetics should have their eyes examined at least once a year.
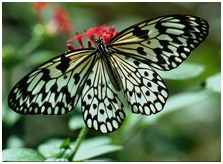
Normal Vision
Blurred image seen when the eyes are affected
How does diabetes affect the eye?
Diabetes produces weakening of the blood vessels in the body. The tiny delicate retinal blood vessels are particularly susceptible. This deterioration of retinal blood vessels, accompanied by structural changes in the retina is termed diabetic retinopathy which leads to loss of vision. Initially the disease is symptomless, ie., patients will have no complaints and they will have perfect vision. But at the same time bleeding or swelling of retina will be taking place. It is treatable only at this stage and this can be identified only on examination by the ophthalmologists. That is why it is important to have the retina examined regularly even if your vision is normal.
Macular Edema
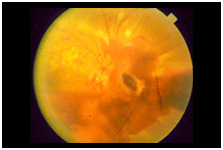
PDR
New blood vessels
rupture and bleed into the vitreous
This causes swelling and exudation in the macula
There are two main causes of vision loss in diabetic retinopathy:
Diabetic Macular Edema: Weakened blood vessels leak and accumulate fluid in the retina causing swelling and exudation in the macula of retina resulting in moderate vision loss.
PDR (Proliferative Diabetic Retinopathy): When new abnormal blood vessels grow or proliferate, bleeding into vitreous may occur with sudden severe vision loss.
Diagnosis
Eye examination in Diabetic Retinopathy
Every diabetic is at risk for developing diabetic retinopathy. Sometimes this can happen even if the blood sugar is kept under good control. There are no symptoms at the initial stages. Periodic eye examination with dilated pupils is the only way to detect diabetic retinopathy in early stage and prevent further deterioration of vision.
Diagnostic tools such as a slit lamp, ultra sound sonography and procedures like fluorescein angiography are used in addition to an ophthalmoscope, to assess the level of diabetic retinopathy.
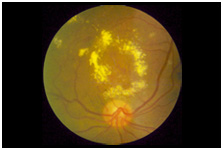
Fluorescein Angiography
This is a magnified photography of the retina using an injectable dye. It helps to stage diabetic retinopathy, record changes in the retinal blood vessels, and to decide on the need and mode of treatment and evaluate the treatment.
Treatment
Lasers are widely used in treating diabetic retinopathy. It is an intense and highly energetic beam of light that can stop or slow down the progression of diabetic retinopathy and improve or stabilise vision.
The laser experience
Laser treatment is usually performed as an out-patient procedure. The patient is given topical anaesthesia to prevent any discomfort and is then positioned before a slit lamp. The ophthalmologist guides the laser beam precisely on the areas to be treated, with the aid of the slit lamp and a special contact lens. Absorption by the diseased tissue either reduces the retinal thickening or stops bleeding. Additional treatment may be required depending on the patients condition.
Side Effects: Some patients may experience side effects after laser treatment. These are usually temporary. Possible side effects include watering eyes, mild headache, double vision, glare or blurred vision. In case of sudden pain or vision loss, the ophthalmologist must be contacted immediately.
REMEMBER
Diabetic retinopathy is often symptomless until the last stage. Once symptoms show up, it is often too late to prevent loss of vision. Hence all diabetics must visit an ophthalmologist once a year to monitor the retina and watch for diabetic retinopathy. Once it is diagnosed, they may need frequent visits to check the progression of the disease with appropriate treatment.
Vitrectomy
In some patients, there may be bleeding into the vitreous or the vitreous may pull on the retina reducing vision severely. These are signs of advanced stages of Diabetic Retinopathy. In such instances a surgical procedure called vitrectomy (replacing the vitreous by a clear artificial solution) is performed.


